Heart Attacks are a Medical Emergency
Angela Boudreau • July 20, 2020
A Heart Attack is an EMERGENCY…Don’t Delay Treatment
At the first sign of a heart attack…call 911. Do not let COVID scare you away from hospitals. Hospitals are, and will remain, the safest place for you to go for an emergency.
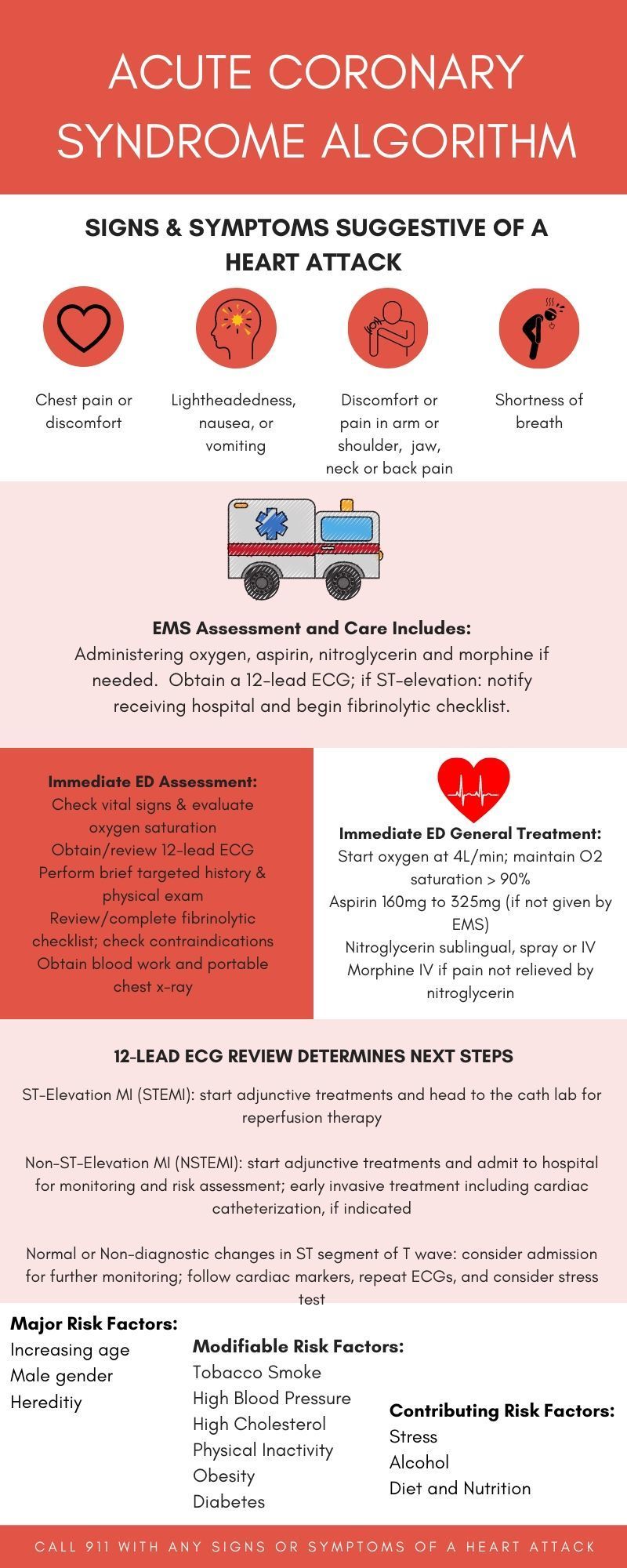
Heart Attack Symptoms:
- Chest discomfort which can feel like pressure, squeezing, fullness or pain
- Pain or discomfort in one or both arms, the back, neck, jaw or stomach
- Shortness of breath
- Cold sweats, nausea or lightheadedness may also be present
Symptoms are sometimes different for women than men. Chest pain or discomfort is the most common sign in men and women, but women are somewhat more likely to experience some of the other common symptoms, such as shortness of breath and back or jaw pain.
Even if you are not certain whether your symptoms could be a heart attack, it is best to get evaluated to know for sure. Time is important, as every minute matters. Do not drive, call 911. An emergency medical services (EMS) team can get treatment started once they arrive, much sooner than for someone who drives by car. Also, patients that arrive to the hospital via EMS are taken directly to a room for treatment. Those that arrive via car must check in at registration and be triaged with the rest of the emergency room patients waiting. For these reasons alone, it is best to call 911.
A heart attack (also called a myocardial infarction, or MI) is caused by heart disease which is the leading cause of death among both men and women in the United States. According to the American Heart Association, each year approximately 785,000 people have their first heart attack and nearly 470,000 of those will go on to have another one.
Heart attacks are usually caused by fatty buildups or atherosclerosis in the arteries. These buildups of plaque narrow the arteries decreasing the blood flow, and thus oxygen, to the heart. If this plaque ruptures it can cause a blood clot to form and further block blood flow. When blood flow is completely blocked to part of the heart muscle, a heart attack occurs. This section of heart muscle without blood flow begins to die. The longer the blood flow is blocked the worse the damage becomes; permeant heart damage and even death can occur.
Want to know if you are at increased risk for a heart attack? The common risk factors are divided into three categories, major, modifiable, and contributing. The more risk factors you have, the greater your risk is.
Major Risk Factors:
- Increasing age
- Male gender
- Heredity (including race)
If your parents have heart disease your risk is increased
African-Americans, Mexican-Americans, American Indians, native Hawaiians and some Asian-Americans are all at a higher risk, partly due to higher rates of severe high blood pressure, obesity and diabetes
Modifiable Risk Factors:
- Tobacco smoke
- High cholesterol
- High blood pressure
- Physical inactivity
- Obesity
- Diabetes
Contributing Risk Factors:
- Stress
- Alcohol
- Diet and nutrition
Treatment for a heart attack varies depending on the type of heart attack you have, although there can be some overlap. The most commonly known types of heart attacks are ST-segment elevation myocardial infarctions (STEMI) and non-ST segment elevated myocardial infarctions (NSTEMI). A STEMI is a very serious form of a heart attack in which a coronary artery is completely blocked and therefore a large part of the heart muscle is unable to receive blood. A NSTEMI is a partial blockage of blood flow to the heart. Commonly used techniques to restore blood flow include clot-busting drugs (thrombolytics), balloon angioplasty (PCI), surgery or a combination of treatments.
A STEMI requires immediate medical treatment. Emergent revascularization is needed to restore blood flow through the blocked artery. Most likely treatment would involve a trip to the cath lab, a department specializing in cardiac catheterization. In the cath lab, a diagnostic angiogram can be done to better examine your heart’s blood flow and how well it is pumping. Depending on these results, a treatment option will be decided: medical management only, percutaneous coronary intervention (PCI), or coronary artery bypass grafting (CABG).
A NSTEMI on the other hand, usually involves one of two treatment options: drug therapy (antiplatelet agents and anticoagulants) to prevent blood clot formation or early invasive treatment starting with drug therapy but also proceeding to PCI with stent placement or CABG.
Dual antiplatelet therapy (DAPT) is also a common treatment among patients post heart attack. This treatment involves two types of antiplatelet medications taken together to prevent blood from clotting. One antiplatelet medication is aspirin. Almost everyone post heart attack is treated with aspirin for the rest of their lives. An additional type of antiplatelet medication, called a P2Y12 inhibitor, is also prescribed for months to years in addition to the aspirin. These P2Y12 inhibitors include clopidogrel (Plavix), prasugrel (Effient), and ticagrelor (Brilinta). The medication type and duration will depend on your specific condition and other risk factors.
If you have a heart attack, make preventing another one your top priority. Most people go on to live a long, productive life. However, about 20 percent of patients 45 years old and older have another heart attack within 5 years of their first.
According to the American Heart Association, here are five things you can do to prevent another heart attack:
- Take your medications as prescribed. Certain medications can greatly lower your risk of another cardiac event. That is why it’s important for you to understand your medications and take them correctly.
- Attend your follow-up appointments. Attending your follow-up appointments will help your doctors keep track of your condition and recovery.
- Participate in cardiac rehabilitation. Cardiac rehabilitation is a medically supervised program designed to help you recover after a heart attack. You should have received a referral to cardiac rehab when you were discharged from the hospital – if you didn’t, ask your doctor about it.
- Manage your risk factors. After a heart attack, it is important to manage risk factors (such as high blood pressure, high cholesterol, and diabetes) by taking your medications, quitting smoking, eating healthier food and getting advice.
- Get support. It is normal to feel scared, overwhelmed and/or confused after a heart attack. Getting support from loved ones or from people who have also experienced a heart attack can help you cope. Connect with other heart attack survivors and caregivers through the American Heart Association Support Network.
A heart attack is a very serious condition and requires fast medical treatment. If you or a loved one think you are experiencing one call 911 and get to the hospital as fast as possible. Do not let COVID or anything else keep you from receiving the life-saving treatment you need.

Telemedicine is not a new concept, however it is newer on the inpatient side. Virtual nurses are slowly being added to the treatment team in hospitals across the country. They are being added as support to the bedside nurse in hopes to alleviate some of the workload and at the same time increase the quality of patient care aa well as patient satisfaction. The nursing shortage, nursing burnout, and the effects of the COVID-19 pandemic are well know to the world of healthcare and beyond. The virtual nurse is hoping to help lessen the impact a bit. While virtual nurses provide extra support to the staff and patients they also provide a much less physically demanding way for experienced nurses to keep working. Many nurses want to be at the bedside and love taking care of patients. This is why they went into nursing in the first place! Unfortunately, nursing is a lot more physically demanding then most people realize. Heavy lifting and constant bending over both take a toll on even the most physically fit nurses. As our nurses age, these demands can become too much. Transitioning into the virtual nurse role could be the perfect alternative. So what exactly can a virtual nurse do in the inpatient setting? There are actually a number of tasks a virtual nurse can assist with. Some of these include reviewing new medications, providing patient education, coordinating communication between the treatment team members, the patient, and family, helping to order meals, helping arrange for discharge transportation and prescriptions, and answering any questions the patient and/or family may have. The virtual nurse is available through the push of a button on the patient room call light and is seen and heard through the patient room TV. To respect privacy, permission is always asked for prior to turning on the camera to see the patient. Also, to ensure quality virtual nurse care, it is a good rule of thumb to only have seasoned nurses on the other side of the camera. The experience of the virtual nurse can be a huge help to a newer bedside nurse. They are a valuable member of the treatment team and can be a mentor too. The virtual nurse helps by ultimately taking away responsibility for many, and sometimes tedious, non-patient care tasks. This frees up the bedside nurse for hands-on patient care. According to Becker's Hospital Review, the US faces a deficit of 450,000 nurses by the year 2025. Can virtual nurses help fill this deficit? While adding virtual nurses to the treatment team may be able to help in many ways, they are not a substitute for the bedside nurse. Some organizations may be hoping to hire fewer nurses overall with the addition of virtual nurses however, they shouldn't take this approach as the quality of patient care cannot be increased with fewer nurses directly at the bedside. The virtual nurse can help fill in many gaps but they cannot provide the same level of care as those physically next to the patient. Organizations need to invest in their nurses and not millions on technology in the hopes of spending less on nurses. No matter how you try to change things up, healthcare cannot survive without nurses. What are the legal implications of virtual nurses in the inpatient setting? Ultimately, the same standards of care exist whether the care provided is virtual or in person. The same tasks have to be completed and the same things have to be documented. Documentation remains key along with communication between team members. Don't assume the other nurse is handling a specific task or documenting an event. Clear roles need to be decided on along with constant communication throughout the shift. This is especially so during the inception of virtual nurses. Change can be difficult and learning how to best utilize virtual nurses will definitely take some time.
Unfortunately, falls with serious injury are consistently among the top ten reported sentinel events. Falls are also preventable. Let's start with some common information about falls: - Mental status and medications are the most significant risk factors for falls. - Falls are common among the elderly, with more than 30% of people 65 and older falling unintentionally. - Head trauma, fractures (including hip), and soft tissue injuries are potential outcomes of patient falls. - Falls can also be fatal. If they aren't fatal, they can lead to permanent disability, a decrease in physical function, and a reduced quality of life. - Falls can also lead to a lose of confidence and an inhibiting fear of falling. These feelings can then lead to further physical decline, depression, feelings of helplessness, and social isolation. - Most falls occur from or near the bed. All patients should be assessed for fall risk: - Ask patients about their fall history. If they have fallen in the past, ask for as much information as possible about the fall. Identifying a pattern can help prevent future falls. Always review the patient's medication list. - Strength, range of motion, pain, posture, and muscle tone should all be assessed. - Objective tests, such as a functional mobility tests and functional gait tests, can help assess a patient's fall risk. A physical therapy consult is usually ideal to evaluate the above mentioned functional mobility and gait tests. However, most tasks can be assessed with close observation and evaluation. -Functional mobility tests rate a patient's ability to do certain tasks, such as sitting or standing unsupported, standing up from sitting, standing with eyes closed, turning, reaching, retrieving an item from the floor, transferring (for example, from chair to bed), and climbing stairs. - Functional gait tests rate the patient's ability to walk. These tests look at how far and how long the patient can walk, how often the patient stops when walking, length and height of the patient's steps, how often and how far the patient strays from a straight path and how much the upper body sways when the patient walks. When indicated, patients should have routine physical therapy to help improve strength and endurance, correct gait and/or balance abnormalities, and improve range of motion. Hospitals should implement fall prevention programs and evaluate the results of such programs. At risk patients and their families should be educated about the risk of falls during hospitalization. They should be taught basic strategies for minimizing risk such as changing position slowly and calling for help. Patients who call for help have fewer falls than those who do not. Reorient confused patients and ask family members to stay with the patient if they can. Confused patients are also best in low beds and near the nurses' station. Unfortunately, with the COVID-19 pandemic and the decreased visitation allowed in many hospitals, the risk of falls in confused patients is much greater. Bed alarms are helpful to alert staff when a patient starts to leave bed. Bed rails and other restraints are sometimes put in place to prevent falls however restraints do NOT reduce the risk of falls and fall-related injuries. In fact, restraints may actually increase fall-related injury and death secondary to limited movement, which leads to muscle weakness and reduced physical function. One routine activity that can play a huge role in patient falls is needing to go to the bathroom. Patients, confused or not, that experience incontinence, urgency or diarrhea, should be checked on and taken to the toilet regularly. This of course also includes patients on laxatives and diuretics (water pills). Hourly rounding is a major standard intervention in most hospitals to help with just this and therefore help prevent falls. Hourly rounding includes checking on every patient at least once an hour and addressing common needs that usually include pain, personal needs, positioning and potty. Since most falls occur near the bed, the following interventions are key. Provide low beds, keep bed brakes locked, make sure the patient can reach all necessary items from bed, keep the bedside free of clutter and do not use all four of the bed rails. As we age every system of our body is affected. These changes can affect our balance and thus increase our risk of falling. - The nervous system responds slower to losses of balance with age. - The musculoskeletal system loses strength and range of motion as we age, which can also affect our balance. - The vestibular system can also lose function with age secondary to peripheral neuropathy and decreased vision. This can affect balance. There are many internal factors that increase fall risk as well: - The cardiovascular system can have a major impact on falls - hypotension (low blood pressure), heart rhythm problems, dizziness, faintness, and lightheadedness are all common causes of falls. - The neuromuscular system is of course another major player in falls - leg or muscle weakness, impaired mobility or loss of movement, poor circulation, unsteady gait, Parkinson's disease, and history of stroke are all huge fall risk indicators. - The musculoskeletal system plays a part too when there is joint pain and/or arthritis which can affect movement and mobility and increase fall risk. - Poor vision and poor hearing thanks to a decrease in the sensory system can lead to increased fall risk as well. - Lastly, the cognitive system plays a tremendous role in fall risk. Confusion, disorientation, intoxication, delirium, Alzheimer's disease and other dementia, as well as chronic mental illness may have the biggest impact on one's fall risk. External factors also play a huge role: - Medications are a major cause, especially psychoactive drugs. These drugs include sedatives, tranquilizers, anti-anxiety drugs and antidepressants. There are plenty of other drugs that may increase fall risk as well, especially if they are new to the patient. These include diuretics, beta-blockers, and any drug that can potentially cause dizziness, unsteadiness, or lowered blood pressure. Patients are also at an increased risk of falling if they take more than four prescription medications. - Environmental factors also play a role. Uneven surfaces, wet or slippery floors, inadequate lighting, clutter, incorrect bed height, poorly fitted or maintained wheelchairs, and a recent environmental change can increase fall risk. If you or a loved one are at an increased risk of falling, make sure the necessary prevention tools are in place. Whether at home or in the hospital, many steps can be put in place to help prevent falling and fall-related injuries. Try to identify the potential causes and look for their solutions or prevention interventions. With the right tools in place, we can all help prevent falls!

While Covid can attack anyone without rhyme or reason, your lifestyle can factor in too. Prevention is key! Practicing good hygiene and working on improving your lifestyle can make a difference. Sadly, Americans aren't exactly know for their healthiness. Our country is full of unhealthy trends, obesity, and sedentary lifestyles. We overeat, overwork, and practice minimal self-care. In order to take care of each other, including our kiddos, parents, and grandparents, we need to first take care of ourselves. While indulgences are definitely okay in moderation, we need to fill our lives with healthy foods and regular activity. Following a healthy lifestyle can naturally boost your immune system and keep you strong and healthy. Here are some basic guidelines to follow. Do not smoke. Eat healthy foods. Exercise regularly. Maintain a healthy weight. Drink alcohol in moderation. Sleep well. Cook meat thoroughly. Minimize stress levels. The immune system requires balance and harmony and can be challenging to boost. Foods rich in antioxidants can help you kickstart this endeavor. Antioxidants such as Vitamins A, C and E are essential to the immune system. These can be found in berries, garlic, and onions, just to name a few. Foods that offer anti-inflammatory properties also boost the immune system. Fruits and vegetables are anti-inflammatory as wells turmeric. So called superfoods are foods that are exceptionally nutrient dense. They are jam packed with vitamins, minerals, and antioxidants which boost cell regeneration and help prevent a multitude of diseases. Some examples of superfoods include berries, dark leafy greens, fish, green tea, whole grains and honey. Here is a more laid out suggestion of foods to help you maintain a healthy diet! Vitamin A (Beta Carotene) - Boosts the health of your intestines and your respiratory system. It is found in carrots, sweet potatoes, spinach, broccoli, and red bell peppers. Vitamin C - Helps stimulate the formation of antibodies. Vitamin C is found in citrus fruits, strawberries, red bell peppers and kiwis. Vitamin E - Promotes the neutralization of free radicals by working as an antioxidant. It is found in vegetable oils, nuts, seeds, and avocados. Zinc - A deficiency in zinc has been linked to immune dysfunction. Boost your zinc levels with beans, seeds, nuts, meat, poultry, and seafood. Protein - Specific amino acids found in protein are essential for T-cell function, which are cells that protect the body against pathogens. Protein is high in meats, poultry, seafood, eggs, beans, nuts and seeds. Eating a good variety of these nutrients will help your immune system work efficiently and effectively. Moderation is also key here, as with most things. Try this variation of one of my favorite immunity boosting smoothies!! 1/2 of a frozen banana 1/2 cup of frozen mixed berries 1 handful of fresh or a cube of frozen spinach 1/4 cup of vanilla greek yogurt 1 dried pitted date 1 tablespoon golden or goji berries 1 tablespoon of almond butter 1/4 teaspoon of ground turmeric 1 crack of black pepper 2 teaspoons of hemp seeds 1 teaspoon bee pollen 1/2 cup unsweetened vanilla almond milk Combine all ingredients, blend until smooth, and enjoy!
The world of healthcare is full of abbreviations. Many are very common while others make you scratch your head and ask yourself, "Did the doctor just make this up?" Some abbreviations may also vary on the medical speciality and/or simply the context of the sentence. This makes abbreviations unreliable and troublesome. Two different people reading the exact same sentence may interpret it completely different because of the abbreviations used. As a result of such confusion, most hospitals restrict the usage of certain abbreviations and The Joint Commission has an official "Do Not Use" list. For example, the abbreviation MS can mean morphine sulfate or magnesium sulfate, two completely different medications. MS can also mean multiple sclerosis. This is just one example. There are many more out there and this is one great reason to have a Legal Nurse Consultant on your legal team. We can help decipher the medical abbreviations and terminology used throughout the medical record. We can help make it all make sense and help you help your clients. Below is a list of common medical abbreviations and a link to The Joint Commission's "Do Not Use" list. ABG = arterial blood gas, measures the oxygen, carbon dioxide, & pH levels in the blood a.c. = before meals ADLs = activities of daily living aFib = atrial fibrillation, an irregular, often fast, heartbeat AKA = above the knee amputation AMI = acute myocardial infarction, heart attack Anuric = not producing urine BID = twice a day BKA = below the knee amputation BP = blood pressure, one of the vital signs CABG = coronary artery bypass graft, open heart surgery CAD = coronary artery disease, heart disease CBC = complete blood count, a common blood test CC = chief complaint CHF = congestive heart failure CNS = central nervous system, includes the brain & spinal cord COPD = chronic obstructive pulmonary disease, a lung disease which makes it hard to breathe CPAP = continuous positive airway pressure, a treatment for sleep apnea CRF = chronic renal failure, kidney failure CVA = cerebrovascular accident, stroke DNR = Do not resuscitate DVT = deep venous thrombosis, blood clot ECHO = echocardiogram, an ultrasound of the heart ETOH = alcohol FX = fracture GFR = glomerular filtration rate, a blood test testing kidney damage gtt = drops H&H = hemoglobin & hematocrit h.s. = at bedtime HTN = hypertension, high blood pressure IM = intramuscular MRSA = Methicillin-resistant Staphylococcus aureus, a drug resistant infection NKDA = no know drug allergies NPO = nothing by mouth NSR = normal sinus rhythm ORIF = open reduction and internal fixation, an orthopedic surgical repair i.e. of the hip PRN = as needed PT = Physical therapy QID = four times a day ROM = range of motion ROS = review of systems, an overall review of the body systems SBO = small bowel obstruction SIDS = sudden infant death syndrome SOB = shortness of breath TIA = transient ischemic attack TID = three times a day TKR = total knee replacement TPN = total parenteral nutrition TURP = transurethral resection of the prostate gland, surgery to remove part of the prostate UA = urinalysis URI = upper respiratory infection UTI = urinary tract infection VSS = vital signs stable https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/do_not_use_list_6_28_19.pdf
If you are a medical malpractice attorney, you know the importance of defining standards of care. You are ultimately trying to prove if the standard was breached or not as it applies to each of your cases. This standard of care lives in the breach of duty when trying to prove professional negligence. The standard of care is how similarly qualified practitioners would have managed the patient’s care under the same or similar circumstances. The standard of care is determined by the expert and based on their education, training, knowledge, and experience. There are many things that influence the standard of care such as practice guidelines, policies & procedures, algorithms & protocols, and the Nurse Practice Act. These all, along with others, come together to create the actual standard of care as defined by the expert in the case. A doctor cannot testify to nursing standards of care, only nurses can. A nurse expert must have a current RN license, be active clinically and/or teaching, have education, training, and experience providing direct patient care and of course knowledge of the standard of care pertinent to the issue(s) in the case. Good communication skills and strong critical thinking skills are also needed. So, while an attorney is working on a medical malpractice case a nurse, and even better a legal nurse, is a great tool to have on board. A legal nurse can help define standards of care. A legal nurse can help organize and explain all of those medical records. A legal nurse can create a timeline or chronology of the events. And, a legal nurse can testify, or find you the best testifying nurse expert. A legal nurse can help you win!
Nurses are often referred to as the heart of healthcare. Our huge hearts, our hard work, our knowledge and our passion to help others hold the healthcare system together. Without nurses there day in and day out advocating and navigating, the healthcare system would fall apart. Nurses do it all! We help care for and coordinate the care of every patient between multiple doctors, multiple disciplines, multiple tests and procedures, and everything in between. We are masters at multitasking and at navigating medical records. You need it, we can find it, or at the very least the person who can. Nurses have a love for life and a love for improving the lives of those we touch. COST-EFFECTIVE: We are comprised of Legal Nurse Consultants (LNCs) who work at much lower rates than medical doctors. Medical doctors charge extremely high fees and they are usually doing this work in addition to their practice which increases their turn-around time. LNCs also serve as expert witnesses and are just as effective as doctors. We are a cost-effective way to identify the strengths and weaknesses of a case. KNOWLEDGE: Legal Nurse Consultants are experts in the healthcare system and have unparalleled experience reading and understanding medical records. As nurses, LNCs have exceptional knowledge of medical terminology and the many subtleties of the healthcare system. We possess a thorough understanding of anatomy, physiology, medical treatment and disease processes. We work in all different areas of healthcare and thus our knowledge is vast. We use this knowledge to analyze medical records to determine if the standards of care were followed or if mistakes were made. We can let you know if the injuries or death were a result of negligence. As LNCs we are also able to modify each case for the attorney, the client, and the jury. HEART: As nurses, we are the heart of the healthcare system and care deeply about our patients. Our main goal is to care for them with the hope they will get better and get to return home. We do know, however, that this is not always how things turn out. As LNCs, we get to take steps to further help our patients when it is needed. We are patient advocates in the hospital and love to get to take that calling further by supporting YOU, their attorneys, in helping them in their time of need. EXPERIENCE: LNCs are nurses first, with a broad area of medical knowledge and experience. Many years of this experience is at the patient's bedside and interpreting their medical records and medical literature. This makes nurses and LNCs ideal for noticing when important documents in the chart are missing or even when they have been tampered with. Nurses, by nature, and especially Legal Nurse Consultants, are very detail oriented and thus will notice things specific to healthcare someone else may miss. This makes LNCs an ideal part of your legal team. RESOURCEFULNESS: At Boudreau Nurse Consulting we belong to a huge network of both medical and professional resources and contacts. If we don't possess the specific specialty needed, we can reach out to one in our network. Our goal is to thoroughly evaluate, analyze and render an informed opinion on the delivery of healthcare and the resulting outcomes.
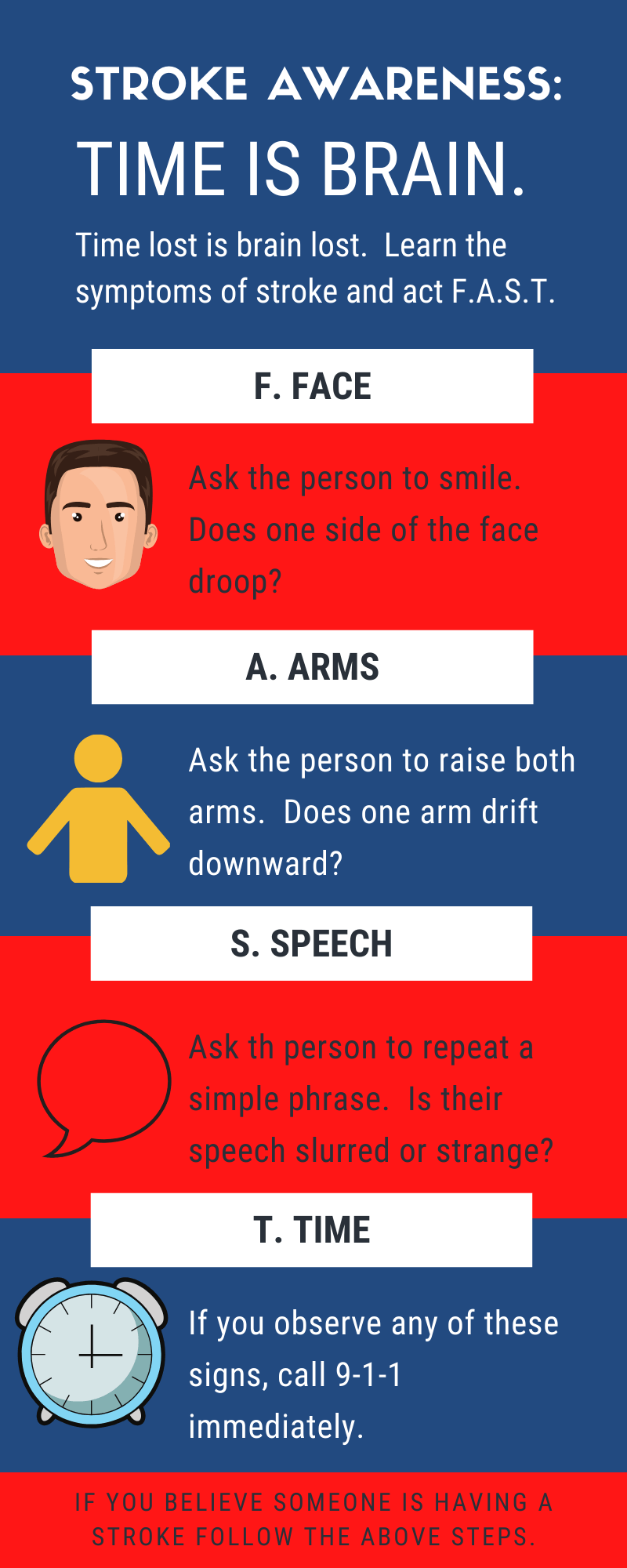
Someone in the United States suffers from a stroke every 40 seconds and these patients are more likely to recover the faster they get treatment. Strokes are largely treatable, as long as such treatment is right away. This is a very important fact that more people need to be aware of. F.A.S.T treatment is Essential! ACT F.A.S.T.: Key Stroke Warning Signs F = Face drooping A = Arm weakness S = Speech difficulty T = Time to call 911 Knowledge of the last well known time is also key as treatment will largely depend on it. If you are with someone when they begin showing symptoms of a stroke call 911 and make note of the time you last saw them well. EMS personal and Emergency Department staff will be asking. Other symptoms to be aware of include a sudden numbness of one's face, arm or leg, especially on only one side of the body. Sudden confusion, understanding or trouble seeing in one or both eyes. Sudden trouble walking, dizziness, loss of balance or coordination. Also, a sudden headache with no known cause. If any of these symptoms come on suddenly call 911 and make note of the last well known time. Due to medical treatment advances, strokes are heading in the right direction. Once fourth it is now fifth amongst the U.S. leading causes of death. Key Emergency Room Treatment Initial hospital treatment should include a head CT, lab work (including PT, INR, CBC and blood glucose), and EKG and a chest x-ray. IV r-TPA Alteplase (TPA) will also be under consideration. TPA is the gold standard clot-busting drug used if there are no contraindications. "Stroke patients who are treated with TPA within 90 minutes of their first symptom were almost three times more likely to recover with little or no disability." The last known well time should at least be within the last 3 hours but sometimes can be extended to 4.5 hours. The head CT must show no signs of bleeding. Past medical history specifically related to bleeding is also taken into consideration. A hemorrhagic stroke (bleeding in the brain) cannot receive TPA and is most commonly caused by uncontrolled high blood pressure. Other essential assessments that should occur early include dysphagia screening, prior to any oral intake, and an NIH Stroke Scale by a stroke certified RN or MD. "In some cases, a procedure to remove the clot causing the stroke is also recommended. Ninety-one percent of stroke patients who were treated with a stent retriever within 150 minutes of first symptoms recovered with little or no disability." Remember, "stroke is largely treatable. It is a matter of getting the right treatment, RIGHT AWAY!"